1. Initial investigation and referral
Your general practitioner (GP) will assess your symptoms. The main symptoms are swollen or painful abdomen, loss of appetite, loss of weight, and night sweats. Your GP will conduct a physical examination and order tests.
Because peritoneal mesothelioma results from the ingestion of asbestos fibres, it is important to mention any asbestos exposure that may have occurred in the past to alert your doctor to this risk factor.
Tests you may have:
- Blood tests: To check your overall health, how your blood cells, liver and kidneys are working.
- X-ray (abdomen and chest): To help identify any abnormalities or fluid build-up in the abdomen and peritoneum, and around the lungs (as the lining of the lungs (the pleura) may also be affected).
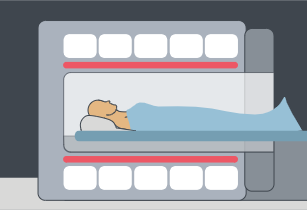
- Computed tomography (CT) scan: Computer technology is used to create detailed images of the abdomen and peritoneum, and the lungs and pleura.
Your GP should also discuss your needs (including physical, psychological, social and information needs) and recommend sources of reliable information and support.
If cancer is suspected, you will be referred to a specialist for further testing. Your GP will provide the specialist with information about your medical history and results of the initial tests.
It can be helpful to bring a family member or friend with you to your appointments.
2. Diagnosis and staging
To determine whether or not you have peritoneal mesothelioma, the specialist will conduct one or more of the following tests:
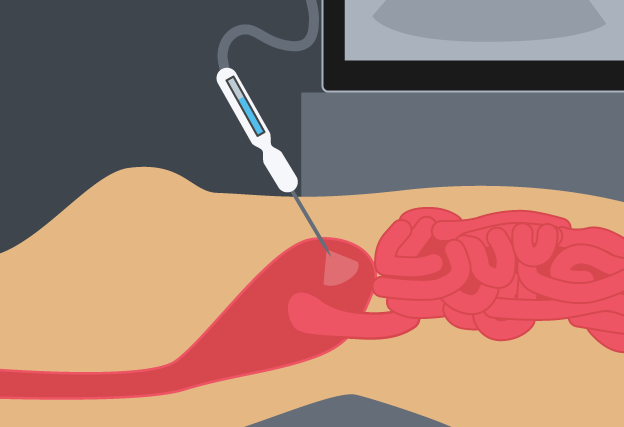
Paracentesis
A sample of fluid from the abdominal area is taken by a needle and sent to a pathologist for testing. This is often performed with the use of ultrasound imaging.
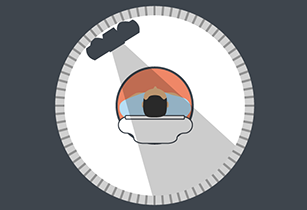
Magnetic resonance imaging (MRI) scan
MRI scans use magnetic fields and radio waves are used to take pictures of inside the body.
Laparoscopy or CT guided biopsy
A small tissue sample (a biopsy) is taken from the abdomen to examine under a microscope. The sample can be taken by keyhole surgery, called a laparoscopy, or using a needle guided by a CT scan.
Positron emission tomography (PET) scan
This produces a three-dimensional image that may show where cancers are located. A small amount of radioactive material is injected and the whole body is scanned.
It can be helpful to contact peer support groups, and support groups for carers.
Here is a list of questions to ask your doctor.
3. Treatment
To ensure you receive the best care, your specialist will arrange for a team of health professionals to plan your treatment based on your preferences and needs. Your specialist will tell you when the team will be discussing your case.
Your team will plan your ongoing care, and should discuss the different treatment options with you including the likely outcomes, possible side effects and the risks and benefits.
You might want to ask for more time before deciding on your treatment, or ask for a second opinion. Your doctor may also suggest you consider taking part in a clinical trial. Let your team know about any complementary therapies you are using or thinking about trying. Some therapies may not be appropriate, depending on your medical treatment.
Treatment options:
Chemotherapy
Chemotherapy is the most common form of treatment. It may be given to try to shrink the cancer or slow its growth.

Surgery
If you have advanced mesothelioma, you may be offered debulking surgery where as much of the cancer is removed as possible. The aim of surgery is to stop the spread of disease and relieve pressure on vital organs.
Peritonectomy (or cytoreductive surgery) may be carried out in certain cases if the cancer has not spread, where the aim is to remove as much, if not all, of the visible tumour.
The surgery may also be combined with the infusion of heated chemotherapy (heated intraoperative intraperitoneal chemotherapy (HIPEC)). This treatment is only carried out by a very small number of surgeons in Australia.

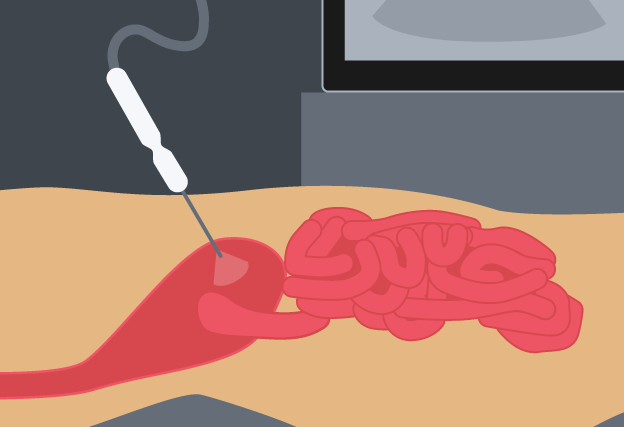
Paracentesis
Paracentesis can provide pain relief in patients with ascites (fluid build-up in the abdomen). A small tube is inserted to allow the fluid to drain out of the abdomen into a bottle.

Watching and monitoring
Often patients have no symptoms either at diagnosis or after the initial surgery. In this case no further treatment is given and your specialist may advise watchful waiting, and dealing with symptoms as they arise.

Your doctor should discuss your needs with you during and after treatment (including physical, psychological, social and information needs) and may refer you to another service or health professional.
4. After treatment
After treatment is completed, your doctor should provide you with a treatment summary that details the care you received, including:
- diagnostic tests performed and their results
- types of treatment used and when they were performed
- treatment plans from other health professionals
- support services provided to you
- contact information for key care providers.
Most patients need to see a specialist for regular follow-ups.
You and your GP will receive a follow-up care plan that tells you:
- the type of follow-up that is best for you
- ways to manage any side effects of treatment, should they occur
- how to get specialist medical help quickly if you think the cancer has got worse.
If you need extra help after treatment, your GP or specialist can discuss your needs with you and refer you to appropriate health professionals and/or community organisations.
5. Living with cancer
Side effects:
Some people experience side effects (for example, tiredness) that continue beyond the end of treatment. Sometimes side effects don’t begin until months after treatment has finished. For more information about side effects ask your doctor.
Advance care plan:
Your doctor may discuss with you the option of developing an advance care plan. An advance care plan is a formal way of setting out your wishes for future medical care. For more information about advance care planning ask your doctor or visit advancecareplanning.org.au.
Palliative care:
This type of treatment could be used at different stages to help you with pain relief, to reduce your symptoms or help improve your quality of life. For more information about palliative care ask your doctor or visit palliativecare.org.au.
6. Questions of cost
There can be cost implications at each stage of the cancer care pathway, including costs of treatment, accommodation and travel. There can be substantial out-of-pocket costs if you are having treatment in a private health service, even if you have private health insurance. You can discuss these costs with your doctor and/or private health insurer for each type of treatment you may have.
Mesothelioma is caused by exposure to asbestos in the majority of cases. If you can identify how you were exposed to asbestos, including from work, you may be eligible for compensation and support. Each state has different schemes for compensation.
You may also be able to initiate a private claim against the responsible company – it is recommended that you contact a specialist asbestos litigation lawyer that deals with such claims.
If you are experiencing financial difficulties due to your cancer treatment you can contact the social worker at your local hospital.
For more information visit costs of treatment.
For more information about accommodation and travel costs visit our support section.
7. Further support
Mesothelioma support
For information about mesothelioma, call Cancer Council on 13 11 20. Specially trained staff at Cancer Council can answer your questions about the effects of cancer, explain what will happen during treatment and link you to support groups and other community resources.
If you need an interpreter, call TIS (the Translating and Interpreting Service) on 13 14 50.
For support and advice for carers, call the Carers Association on 1800 242 636.
More support options
Australian Cancer Survivorship Centre
Has general and tumour-specific information, primarily focused on the post-treatment survivorship phase
• Telephone: (03) 9656 5207
• Website: www.petermac.org/cancersurvivorship
National Health Services Directory
A directory providing information on local hospital and community services
• Website: www.nhsd.com.au
Asbestos Diseases Research Institute
Provides information on Mesothelioma and referral to support groups and programmes.
• Telephone: 1300 237 400
• Website www.adri.org.au
beyondblue: the national depression initiative
Information on depression, anxiety and related disorders, available treatment and support services
• Telephone: 1300 22 4636
• Website: www.beyondblue.org.au
Cancer Australia
Information on cancer prevention, screening, diagnosis, treatment and supportive care for Australians affected by cancer, and their families and carers
• Telephone: 1800 624 973
• Website: www.canceraustralia.gov.au
The Bernie Banton Foundation
Information on mesothelioma, available treatment and support services.
• Telephone: 1800 031 731
• Website: www.berniebanton.com.au
Care Search: Palliative Care Knowledge network
Information for patients and carers on living with illness, practical advice on how to care, and finding services
• Telephone: (08) 7221 8233
• Website: www.caresearch.com.au
Optimal care pathways have been developed for health professionals and health services. However, patients and carers may find useful information in this version to help understand the processes their treating health professionals are following.

